July 15, 2020
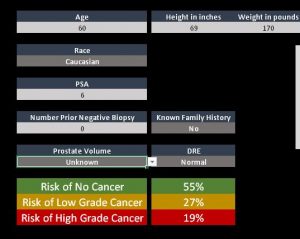 A new prostate cancer risk calculator developed by Kaiser Permanente Northern California researchers may help men going through prostate cancer screening make the difficult decision of whether or not to have a prostate biopsy. The calculator predicts the likelihood that a patient with an elevated prostate-specific antigen (PSA) test or abnormal digital rectal exam will have a biopsy that shows no cancer, a low-grade cancer, or a high-grade cancer.
A new prostate cancer risk calculator developed by Kaiser Permanente Northern California researchers may help men going through prostate cancer screening make the difficult decision of whether or not to have a prostate biopsy. The calculator predicts the likelihood that a patient with an elevated prostate-specific antigen (PSA) test or abnormal digital rectal exam will have a biopsy that shows no cancer, a low-grade cancer, or a high-grade cancer.
“The PSA is not a great test because an elevated result doesn’t mean you have cancer, and even if you do it might be a low-grade cancer that will never grow any larger,” said Joseph Presti, MD, the Regional Leader of Urologic Oncology Surgery with The Permanente Medical Group and an adjunct researcher at the Kaiser Permanente Northern California Division of Research. “With the calculator, the doctor can plug in information about the patient — age, race, family history for prostate cancer, body mass index, PSA level, number of prior negative biopsies, result of the rectal exam, prostate volume — and get results that can help the patient determine whether to undergo additional tests or have the biopsy.”
A paper describing the new calculator and the accuracy of its risk prediction models is now online in the journal Urologic Oncology. The American Cancer Society estimates that this year approximately 192,000 men will be diagnosed with prostate cancer and about 33,000 will die from the disease in the U.S. For more than a decade, researchers have debated whether men should have an annual PSA test to screen for prostate cancer. The debate over the test centers on whether the risk of overdiagnosis —treating men for cancers that would never have caused serious medical problems — outweighs the benefit of finding an aggressive cancer before it can become deadly.
“Prostate cancer screening has been an enormous problem for many years,” said the study’s senior author Andrew L. Avins, MD, MPH, a research scientist at the Division of Research. “It’s very confusing for providers and patients. By leveraging our large database at Kaiser Permanente, we sought to create a better tool to help patients and providers determine the value of pursuing a diagnosis after an elevated PSA.”
In 2012, the United States Preventive Services Task Force (UPSTF) issued new guidelines that recommended against the use of PSA testing. In 2018, the USPSTF revised its guidelines, recommending that men age 55 to 69 discuss the benefits and risks of PSA testing with their doctors and make a decision based on their values and preferences. The Kaiser Permanente researchers who developed the new calculator published research in 2019 that showed an increase in metastatic prostate cancers diagnoses after the USPSTF discouraged testing in 2012. This finding, also seen in other studies, supports the use of shared decision-making.
“What we want,” said Dr. Presti, “is for the calculator to hopefully decrease the number of men who undergo biopsy and thus decrease the number of slow-growing cancers detected that we would rather not find. We also want to decrease the number of men who have multiple biopsies that do not show cancer. Ideally, we would only perform a biopsy on men with a significant risk of having an aggressive cancer that needs treatment.”
The new calculator is the first to have been developed using a racially diverse population, and the information it provides reflects racial and ethnic disparities in prostate cancer
incidence and death. Prostate cancer is less common in Asian American and Latino men than it is in white men. Black men are more likely than men of other races and ethnicities to be diagnosed with — and 2.5 times more likely to die of — prostate cancer than non-Hispanic white men. They also are more likely to develop prostate cancer at a younger age. These findings support more aggressive screening for Black men.
To create the calculator, the researchers collected data on the race/ethnicity, family history of prostate cancer, findings from a digital rectal exam (if done), number of previous biopsies, and prostate volume of 2,967 men who had a biopsy between May 2016 and November 2017. They then developed statistical models that incorporated various factors from the men’s medical and family histories to predict the chance of a biopsy showing no cancer, a low-grade cancer, or a high-grade cancer. The models are now being tested in another group of 3,000-4,000 Kaiser Permanente patients who had a biopsy following an elevated PSA or abnormal digital rectal exam. Findings from this study are expected to be published within the next year.
The researchers hope to conduct a prospective study that will assess whether patients and providers find the calculator helps them in their decision making. “Based on our initial work, it looks like this tool could help patients make more personally relevant decisions about whether to have a biopsy to look for prostate cancer,” said Avins. “These are heavily value-laden decisions. Our goal is to reduce a patient’s uncertainty and to help them make decisions that are more in line with their preferences and values.”
The study was funded by The Permanente Medical Group’s Delivery Science and Physician Researcher Programs.
Co-authors included Stacey Alexeeff, PhD, Brandon Horton, MPH, and Stephanie Prausnitz, MS, of the Division of Research.
This story originally appeared in Division of Research Spotlight