November 20, 2020
When Mariann Stephens, 44, a first-grade teacher and mother of 2 from Pleasanton, California, learned she had lung cancer, she couldn’t believe it.
“I’ve never smoked in my entire life,” Stephens said. “This was a total curveball. You don’t expect to be told you have cancer at my age.”
Lung cancer is by far the leading cause of cancer death in the United States. While cigarette smoking is the number one risk factor for lung cancer, according to the American Cancer Society, about 1 in every 5 people who die from lung cancer have never smoked or used tobacco.
“A curse and a blessing”
Stephens’ story began on Valentine’s Day 2013, when she came down with severe pneumonia and was hospitalized for a week. The pneumonia left substantial scarring on both lungs, and her doctors recommended annual screenings to monitor the impact of the scarring.
After years of surveillance, a CT scan showed that a small nodule on her right lung had changed and grown.
“It turns out the pneumonia was both a curse and a blessing,” said Stephens. “If it weren’t for my pneumonia, I wouldn’t have been going in for annual scans, and the nodule could still be growing inside me. I feel like I dodged a huge bullet.”
Combining diagnosis and treatment
Stephens was referred to Jeffrey Velotta, MD, a thoracic surgeon for The Permanente Medical Group, to discuss her treatment options. Dr. Velotta recommended a surgical procedure that would allow him to take a small tissue sample and test it for cancer immediately, getting the results while Stephens was still on the operating table.
“It’s diagnosis and treatment at the same time,” said Dr. Velotta, who practices at the Kaiser Permanente Oakland Medical Center. “Nodules like this are often hard to diagnose because they’re so small, but our lung cancer program has a system in place where I can send a sample downstairs to a specialist in lung pathology and get a 99% accurate diagnosis in less than 30 minutes.”
The test showed that the nodule was indeed cancerous, so Dr. Velotta removed the upper right lobe of Stephens’ lung and affected lymph nodes using video-assisted thoracoscopic surgery, or VATS. This minimally invasive technique allows for much smaller incisions in the chest wall, resulting in lower complication rates and less postoperative pain.
“I’m so thankful he was able to do everything in one shot,” said Stephens. “It saved me unnecessary steps and extra procedures. They were able to remove all the cancer, so I didn’t need chemo or radiation.”
“I owe him my whole life”
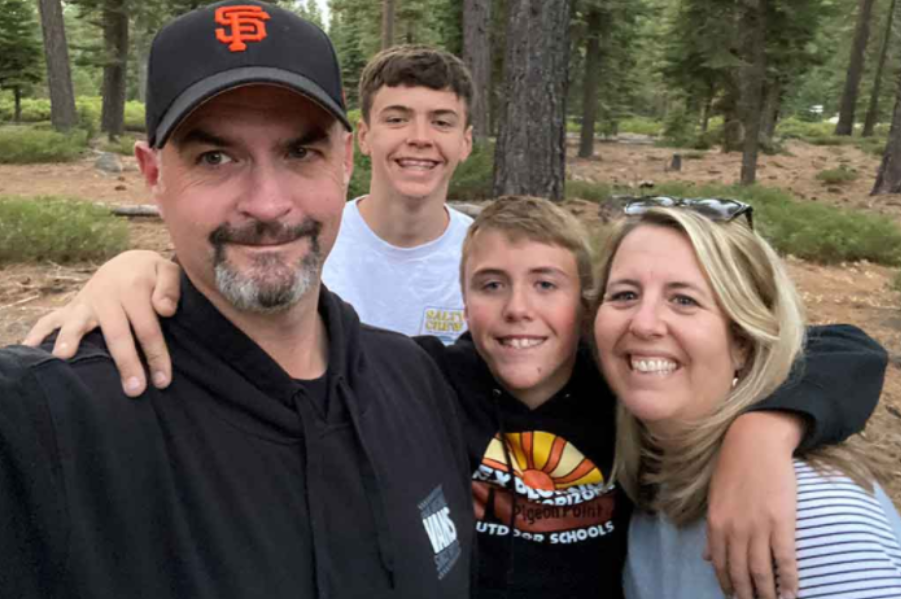
Stephens is now cancer-free and healing well. She recently spent time near Lake Tahoe with her family, taking walks and enjoying the fall scenery.
“Dr. Velotta told me I should be back to normal soon, and that I’ll be able to explore the beautiful Sierras and do all the other fun things I’ve always done,” she said.
“He’s my hero. I owe him my whole life.”
This story originally appeared in About Kaiser Permanente