August 2, 2021
The experience and expertise cultivated within a regionalized, virtual gastric cancer center can improve outcomes for stomach cancer patients by making it faster and easier to introduce leading-edge cancer treatments, a new Kaiser Permanente study shows.
The research, published August 2 in the Journal of Clinical Oncology, is believed to be the first U.S. paper to describe the impact of a regionalized gastric cancer care program.
“Overall, the number of people who develop stomach cancer in the U.S. is quite small,” said the study’s lead author Swee H. Teh, MD, surgical director for Gastric Cancer Surgery with The Permanente Medical Group. “Before we regionalized care, an oncologist in a Kaiser Permanente Northern California hospital might see only a few stomach cancer patients a year. Patients would have an open surgery, and typically a longer hospital stay. Now, we have a highly specialized surgical group that performs minimally invasive surgery with a more extensive lymph node dissection. We believed this approach, along with other aspects of regionalization, would improve patient care, and the findings from this paper are the first evidence showing that this is the right path.”
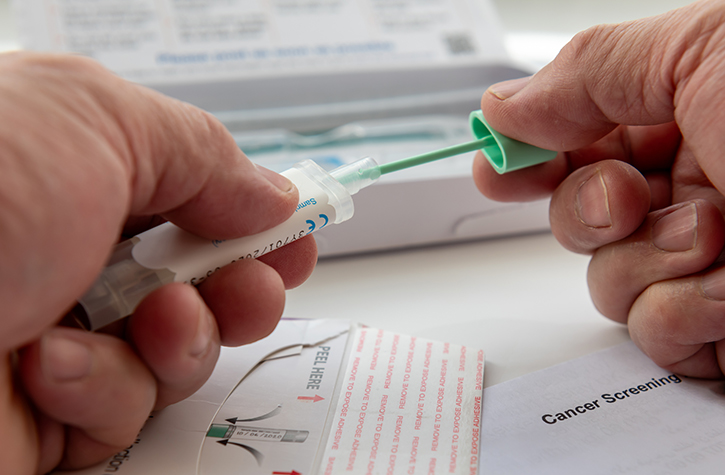
Since the Kaiser Permanente Northern California (KPNC) Gastric-Esophageal Cancer Program was established in 2016, each patient has had their medical tests reviewed by a team of 7 experts who determine the best treatment approach. Those who require surgery have the procedure performed at one of the 2 KPNC Gastric Surgery Centers of Excellence. The chemotherapy regimen selected by the expert team is given at the hospital closest to the patient’s home. A Patient Care Coordinator serves as the primary liaison between the program and the patient to ensure timely, coordinated care.
“This program ensures every patient with potentially curable gastric-esophageal cancer receives the highest quality multidisciplinary care from our region’s top subspecialty experts,” said medical oncologist Yan Li, MD, PhD, who co-leads the regional program with medical oncologist I-Yeh Gong, MD.
The American Cancer Society estimates that about 26,560 people in the U.S. will be diagnosed with stomach cancer, also known as gastric cancer, this year. This represents about 1.5% of all new cancer diagnoses. According to the California Cancer Registry, about 3,000 stomach cancer diagnoses now occur in the state each year.
“In our entire region, which serves about 4.5 million members, we see about 200 gastric cancer patients per year,” said Li. “Our specialized team brings the expertise we develop from seeing this volume of patients to the care we provide.”
The retrospective study included all 1,429 KPNC members diagnosed with stomach cancer between January 2010 and May 2018. The study compared the outcomes of the 942 patients diagnosed before the regional gastric cancer team was established in 2016 with the outcomes of the 487 patients treated after it was implemented. The researchers also took a closer look at the 715 patients — 443 treated before regionalization, 272 treated after — with a stage I, II, or III cancer who had surgery to remove the tumor. Before regionalization, survival rates among this group were 73%; after regionalization, they rose to 86%.
“The regionalized gastric cancer program combines the benefits of community-based care, which is local and convenient, with the expertise of a specialized cancer center,” said co-author Lisa Herrinton, PhD, a research scientist at the Kaiser Permanente Division of Research. “It is also an example of one of the strengths of Kaiser Permanente. In our integrated care system, it is easy for the different physicians that treat cancer patients — surgical oncologists, medical oncologists, and radiation oncologists, among others — to come together and collaborate and tie their work flows together.”
Regionalizing care made it possible to introduce new surgical procedures. “We now treat patients with less-invasive laparoscopic surgical techniques and perform more comprehensive lymph node dissections,” said Teh. This surgical approach is used widely in many Asian countries with high rates of stomach cancer. Still, it has not yet become common in the U.S. “We have proven that these techniques are safe and that they improve outcomes for Western patients as well,” he added.
Regionalizing care also made it possible for medical oncologists to uniformly introduce and standardize the use of the newest chemotherapy regimens. “Cancer care is becoming increasingly complex,” said Li. “By creating a program of subspecialists, we can provide leading-edge treatments for our patients. This is a patient-driven cancer model that is both high quality and convenient.”
Adds Teh, “Our program gives a glimpse of what is possible in gastric cancer care. We are setting the bar higher, for ourselves and others.”
This study was funded by The Permanente Medical Group Delivery Science and Applied Research program.
Co-authors include Stephen Uong, MPH, and Teresa Y. Lin, MPH, of the Division of Research, and Sharon Shiraga, MD, and Robert A. Li, MD, of The Permanente Medical Group.
This article originally appeared in Division of Research Spotlight