February 23, 2022
Kaiser Permanente Northern California program eliminated disparities in colorectal cancer death rates between Black and white members
Colorectal cancer disparities between Black and white adults were eliminated in Kaiser Permanente Northern California members after the health care system instituted a regionwide, structured colorectal cancer screening program, new research shows.
“Our study found that organized screening works to improve colorectal cancer outcomes for all of our members,” said the study’s senior author Theodore R. Levin, MD, a research scientist at the Kaiser Permanente Northern California Division of Research and a gastroenterologist with The Permanente Medical Group. “I knew our program had helped to reduce disparities, but I was surprised by the magnitude and the rate of improvement. It exceeded my expectations.”
Disparities between Black and white adults in colorectal cancer screening, incidence, and death rates have been documented for more than 40 years. Screening programs create an opportunity to find colorectal cancers when they are small and easier to treat. Screening can also prevent cancers from developing through the removal of precancerous polyps.
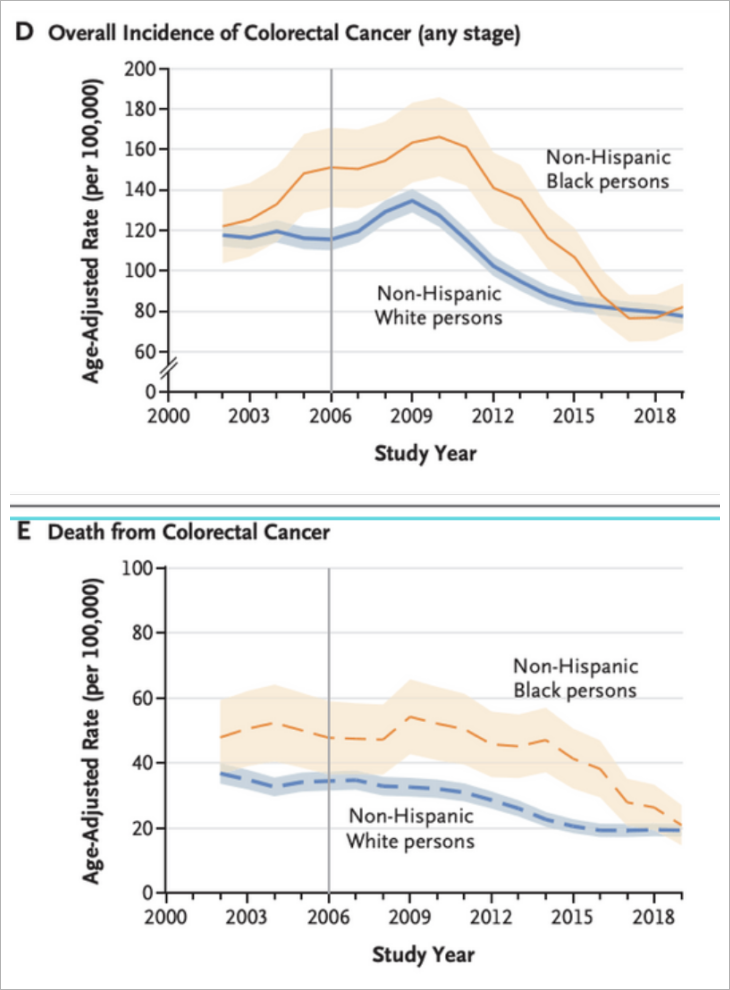
The new study, published February 24 in the New England Journal of Medicine, looked at colorectal cancer screening participation, incidence, and death rates for Black and white KP Northern California members ages 50 to 75 from 2000 through 2019. The 19-year time period spanned 6 years before and 11 years after the program’s implementation in 2006 through 2008.
In 2009, the colorectal cancer death rate (per 100,000) was 54.2 for Black members and 32.6 for white members. By 2019, death rates had fallen by more than half among Black members — decreasing to 20.9 — compared to 19.3 for white members, essentially eliminating the previous disparity. Colorectal cancer incidence also markedly decreased with similar rates seen between Black and white members.
“It is inspiring that organized screening outreach markedly and rapidly increases screening for everyone,” said the study’s co-lead author Douglas A. Corley, MD, PhD, a research scientist at the Division of Research and a gastroenterologist with The Permanente Medical Group. “This is a powerful message that organization is crucial for knowing when and how to engage members in screening and follow-up.”
The findings highlight the need for health care systems to address the social and structural barriers that contribute to ongoing health disparities. “Many people have sought to show that health equity is not just a pipedream,” said the study’s co-lead author Chyke A. Doubeni, MBBS, MPH, who directs the Mayo Clinic Center for Health Equity and Community Engagement Research. “This study shows how a thoughtful, intentional, coordinated, and sustained approach to delivering care in an equitable manner can eliminate health disparities.”

Chyke Doubeni, MBBS, MPH, Director, Mayo Clinic Center for Health Equity and Community Engagement Research.
The colorectal cancer screening program identifies who needs screening and offers a choice of screening tests. Program managers and electronic systems identify all eligible members who are not up to date and automated alerts remind health care providers to offer screening at clinic visits. For members who are not up to date with screening, a fecal immunochemical test (FIT) is mailed annually. These tests can easily be completed at home and returned by mail. Patients can request a colonoscopy, rather than use the FIT kit.
After starting organized screening outreach, the proportions of people up to date with screening rapidly increased, from about 40% among both Black and white KPNC members in 2009 to 80% among Black members and 83% among white members by 2019.
 “Screening doesn’t stop with the delivery of the mailed fecal immunochemical test,” said Dr. Levin. “Ensuring people complete the screening and ensuring those who are positive complete a colonoscopy and, if needed, cancer treatment are all important parts of our program. We are also intentional to make sure our screening materials are culturally competent and address issues important to marginalized communities. This includes addressing concerns about trust in the health care system as well as making the connection between screening and being present for your family.”
“Screening doesn’t stop with the delivery of the mailed fecal immunochemical test,” said Dr. Levin. “Ensuring people complete the screening and ensuring those who are positive complete a colonoscopy and, if needed, cancer treatment are all important parts of our program. We are also intentional to make sure our screening materials are culturally competent and address issues important to marginalized communities. This includes addressing concerns about trust in the health care system as well as making the connection between screening and being present for your family.”
The study was funded by the National Cancer Institute.
Co-authors include Wei Zhao, MPH, and Christopher D. Jensen, PhD, of the Division of Research; and Chyke A. Doubeni, MD, MPH, and YanKwan Lau, PhD, MPH, of the Mayo Clinic.
This article originally appeared in Division of Research Spotlight.