March 23, 2022
Kaiser Permanente study finds reversal of prior national trends and widening racial disparities
Deaths from heart disease and stroke in the U.S. due to factors other than an aging population increased during the first year of the COVID-19 pandemic, reversing prior trends and widening racial and ethnic disparities, new research shows.
“We expect the number of deaths from heart disease and stroke to go up every year because the number of people 65 and over in the U.S. is increasing, and this is the group most likely to die from these conditions,” said the study’s lead author Stephen Sidney, MD, MPH, a senior research scientist at the Kaiser Permanente Northern California Division of Research.
“We had been making progress in reducing deaths from heart disease and stroke due to preventive measures and timely interventions,” Sidney said. “Our study showed the pandemic didn’t just stop these gains, it reversed them, with Black, Latino, and Asian adults hit hardest.”
The study, published March 23 in JAMA Network Open, analyzed national mortality data collected by the Centers for Disease Control and Prevention.
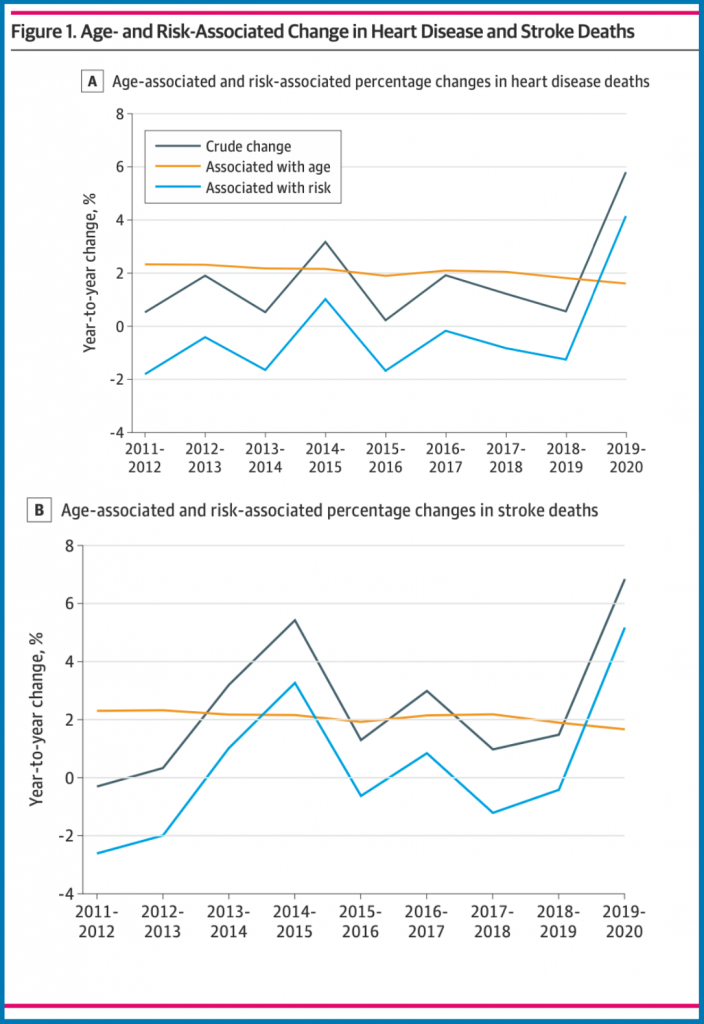
The researchers used statistical techniques that allowed them to account for the aging population as they compared heart disease and stroke deaths in the 8 years prior to the pandemic (2011-2019) with those that occurred in the first year of the pandemic (2019-2020).
The analyses showed that during the first year of the COVID-19 pandemic, deaths from heart disease due to risk factors other than an aging population grew by 11.9% in Black adults, 11.2% in Latinx adults, 9.9% in Asian-Pacific Islanders, and 2.3% in white adults.
Similar disparities were seen in deaths from stroke not accounted for by an aging population, where deaths increased by 8.9% in Black adults, 7.4% in Latino adults, 7% in Asian adults, and 4.2% in white adults. Black adults had both the greatest increase and the highest overall rate of heart disease and stroke deaths.
The scope of the study couldn’t pinpoint the precise reasons for the rapid spike. But the research team said the impact the pandemic had on the health care system and overall access to care likely played a big role.
“Nationwide we were seeing overcrowded hospitals due to COVID-19,” said the study’s senior author Jamal S. Rana, MD, PhD, an adjunct investigator with the Division of Research and a chief of cardiology with The Permanente Medical Group. “We also know that COVID-19 itself can have a deleterious effect on heart disease and strokes, what is alarming is the disproportionate impact.”
Dr. Rana continued, “It is as if the pandemic melted the tip of the iceberg to reveal how precarious the health care situation is for Black, Latino, and Asian adults in the U.S. These data are more evidence pointing to the underlying structural racism, systemic inequities, and social determinants of health that create different outcomes in communities of color.”
Co-authors include Catherine Lee, PhD, Jennifer Liu, MPH, of the Division of Research; and Sadiya S. Khan, MD, and Donald M. Lloyd-Jones, MD, ScM, of Northwestern University.
This article originally appeared in Division of Research Spotlight.