December 29, 2023
An electronic reminder to recommend smoking cessation therapy to hospitalized patients substantially increased the number of people getting therapy and was related to a 5% increase in patients who said they stopped smoking tobacco.

Somalee Banerjee, MD, MPH
In a study published in BMJ Open, Kaiser Permanente Northern California researchers described a project that added a physician prompt to the electronic health record (EHR) recommending nicotine replacement therapy – patches or gum – when a smoking patient is admitted or discharged from the hospital.
The initiative resulted in a significant increase in the number of patients prescribed nicotine replacement therapy, going from 30% in the year before the electronic reminders were added, to 78% in the year after. The study also found a 5% increase in the number of patients who reported quitting smoking in the 30 days after they left the hospital.
“This reminder comes up on the screen for our hospitalists for each of these patients,” said lead author Somalee Banerjee, MD, MPH, a hospitalist physician with The Permanente Medical Group. “It is a simple intervention that any hospital or health system could use, just stopping clinicians for a second at admission or discharge to click on nicotine replacement therapy and make it easy for them. We wanted to find out whether the intervention was making a difference for patients.”
The “hard stop” reminders were added to the EHRs at 21 Kaiser Permanente Northern California hospitals in 2015; clinicians admitting or discharging a patient would need to either manage the established set of orders or bypass it. The study authors examined 20,847 patient encounters in the year before the initiative began and 20,958 patient encounters in the year after.
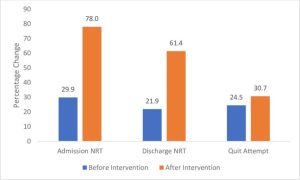 About 11% of the patients already had a prescription for nicotine replacement. Before the reminders began, 30% of smoking patients received a prescription order on hospital admission, and 78% received one after.
About 11% of the patients already had a prescription for nicotine replacement. Before the reminders began, 30% of smoking patients received a prescription order on hospital admission, and 78% received one after.
Because most hospitalized patients in the Kaiser Permanente integrated health system had an outpatient follow-up visit in the following month, the researchers were able to track their smoking status. The analysis found a 5% increase in the number of patients who self-reported that they had quit smoking.
“The hospital admission setting is a good time for people to start quitting because they are not going to be smoking while they are hospitalized, and they may be having some kind of major health issue that makes them rethink their health choices,” Dr. Banerjee said.

Kelly Young-Wolff, PhD, MPH
“Our universal approach to offering nicotine replacement therapy to all hospitalized patients who smoke can help to reduce disparities,” said senior author Kelly Young-Wolff, PhD, MPH, a clinical psychologist and research scientist at the Kaiser Permanente Northern California Division of Research. “This type of health care system-based intervention can help ensure equity.”
The study was funded by the Kaiser Permanente Northern California Community Health grants.
Additional co-authors were Amy Alabaster of the Division of Research; Renee Fogelberg, MD, and Nihar Patel, MD, of Kaiser Permanente Oakland Medical Center; and Alyce S. Adams, PhD, of Stanford University.
This article originally appeared in Division of Research Spotlight.






