March 5, 2024
HIV prevention medication is highly effective in preventing new HIV infections in people at high risk, but it doesn’t reach most people who could benefit. Kaiser Permanente researchers and doctors with The Permanente Medical Group designed a targeted messaging system to alert primary care physicians before a visit with a patient who might be at risk for contracting HIV so they can discuss prevention.

Michael Silverberg, PhD, MPH
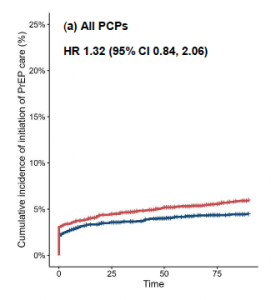
A randomized trial to test the system found that receiving a single message from a medical staff member resulted in a significant increase in referrals for preexposure prophylaxis (PrEP) by primary care doctors who also see people with HIV as part of their practice. But it did not increase referrals among primary care doctors who do not have experience caring for those with HIV. Results were published in the journal JAIDS.
“The intervention worked very well for primary care physicians who are already focused on patients with HIV,” said senior author Michael Silverberg, PhD, MPH, an investigator with the Kaiser Permanente Division of Research (DOR). “But for other primary care physicians, this one email was not enough to increase PrEP referrals, which may have been a result of other competing demands during relatively brief clinic visits. We learned that for these providers, a relatively light-touch intervention such as a single staff message may not be enough.”
The trial tested a clinical decision support intervention — an email alert via a secure staff messaging system — that alerted clinicians about upcoming visits with patients predicted to be at high risk for acquiring HIV. The risk evaluation was based on information from a previously validated prediction model, whose development was led by coauthor Julia Marcus, PhD, MPH, an infectious disease epidemiologist at Harvard Medical School and former DOR research fellow. The model used more than 40 data elements from the Kaiser Permanente electronic health record to identify patients at higher risk for HIV acquisition.
PrEP therapy effectively reduces the chances of contracting HIV and can be taken daily, by injection, or on an on-demand basis during periods of risk. It is estimated that just 30% of people at risk for HIV use PrEP, and public health officials have struggled to reach people at the highest risk.
Incorporating PrEP messaging
 The researchers designed the messaging system to take into account busy physicians’ schedules and the number of electronic alerts they already receive about a variety of topics. The message provided information and resources about PrEP, identified that the patient may benefit from HIV prevention services, and provided instructions for referral for PrEP care. The message did not include details regarding the actual calculated risk level or what data elements were used to determine the patient’s score.
The researchers designed the messaging system to take into account busy physicians’ schedules and the number of electronic alerts they already receive about a variety of topics. The message provided information and resources about PrEP, identified that the patient may benefit from HIV prevention services, and provided instructions for referral for PrEP care. The message did not include details regarding the actual calculated risk level or what data elements were used to determine the patient’s score.
The study team recruited 121 primary care doctors in San Francisco and split them into 2 groups, one receiving the intervention emails, and the remainder providing usual care. The physicians included a dozen who already had people with HIV among their patients; these doctors were split equally between the 2 study groups.
The trial ran between June and November 2021 and involved 5,051 patient appointments. The researchers tracked PrEP care initiation which could include PrEP discussions, referrals to a dedicated PrEP care team, and PrEP prescriptions.
Jonathan Volk, MD, MPH
They found a slight but statistically insignificant increase in PrEP care initiation among doctors receiving the email prompts (6% vs. 4.5%). However, among the primary care providers who regularly see patients with HIV, there was a significant 2.5-times higher rate of PrEP referrals for those in the intervention compared with usual care.
“It’s possible the primary care doctors who do not care for people with HIV need more information about the specific patient’s risk factors to understand why they would need to raise a discussion about HIV prevention at the visit,” said lead author Jonathan Volk, MD, MPH, an infectious disease specialist with The Permanente Medical Group. “They may also not have as much experience and comfort navigating discussions about sexual health, particularly with men who have sex with men.”
Continued innovation planned
Since the decision support trial, additional tools have become available to reach people who could benefit from PrEP, Volk said. For instance, Kaiser Permanente (KP) Northern California has initiated an electronic self-referral visit for sexual health that could reach patients at risk for HIV who are not comfortable having sexual health discussions with their doctors. The research team plans to continue looking for innovative ways to use their prediction model to reach patients who could benefit from PrEP, Volk said.
The predictive model was developed previously by the study team using data from the KP Northern California health system. Previous research has shown the model to be more effective than other HIV risk prediction models, including better discrimination of HIV risk across all races and ethnicities. In coordination with KP Northern California’s predictive analytics team, led by co-author Vincent Liu, MD, a DOR research scientist, the researchers computed risk scores based on the prediction model directly within the Kaiser Permanente electronic health record. This allowed for real-time evaluation of risk for HIV and timely staff messages to providers with upcoming clinic visits with patients at risk for HIV.
“This study evaluated how artificial intelligence can be use in a busy primary care practice to increase access to HIV PrEP, a highly effective intervention with limited and inequitable uptake,” Dr. Volk said.
The study was funded by The Permanente Medical Group’s Delivery Science and Applied Research Program.
Additional co-authors were Catherine Lee, PhD, Wendy A. Leyden, MPH, and Alexandra N. Lea, MPH, of the Division of Research; Michelle C. Donnelly, BA, of Kaiser Permanente Information Technology; Douglas S. Krakower, MD, of Beth Israel Deaconess Medical Center; and Kristine Lee, MD, of The Permanente Medical Group.
This article originally appeared on Division of Research Spotlight.






