Surgeons in The Permanente Medical Group are offering jaw reconstruction and dental restoration in a single surgery, shrinking a one-to-two-year timeline to a day.
August 12, 2025
The first patient in Kaiser Permanente Northern California to undergo total maxillofacial reconstructive surgery, also known as Jaw-in-a-Day, was a young woman missing all her lower right teeth.
More than a decade earlier, as an early teen, she’d had surgery at another health care institution to treat a large benign tumor in her jaw. The procedure involved a segmental resection of her mandible — removing both the tumor and a portion of the bone — along with the attached teeth. Her jaw was then reconstructed using a bone graft from her hip and stabilized with a metal plate.
After healing, however, the patient did not pursue the two subsequent oral reconstructive surgeries that were required to place a dental prosthesis. Instead, she adapted to life with incomplete dentition and its associated challenges, including impaired chewing, speech difficulties, and self-consciousness, assuming this would always be her reality.
Then last November, the plate in her jaw fractured without warning, resulting in the failure of her jaw reconstruction. Now a Kaiser Permanente member living in the North Bay, the 29-year-old woman sought urgent medical care and was swiftly referred to the Head and Neck Surgery Department at KP Oakland.
“When this patient came to see me, I felt so bad for all that she’d been through,” says Deepak Gurushanthaiah, MD, head and neck surgeon and microvascular surgeon with The Permanente Medical Group. “I conferred with my colleagues, and we agreed: It was time to make Jaw-in-a-Day happen — not only for this patient, but for any eligible patient in KP Northern California who needs it. She was the perfect candidate for our first case.”
Waking up with a smile

Deepak Gurushanthaiah, MD
Total maxillofacial reconstructive surgery, or Jaw-in-a-Day, represents a quantum leap in care for patients who have benign or malignant tumors of the mandible or maxilla and require complex ablative and reconstructive jaw surgery. More rarely, this surgery may also be indicated for patients with jaw trauma or infection.
“With Jaw-in-a-Day, we’re taking multiple surgical procedures that traditionally happen sequentially over a one-to-two-year period, and instead performing them in parallel during a single episode of care,” says Dr. Gurushanthaiah. “So in one orchestrated operation, not only do we remove the jaw tumor and rebuild the jaw with a vascularized bone graft, but we also insert titanium dental implants into the graft and place a customized provisional dental prosthesis. This means that the patient wakes up from surgery with teeth that look like their own.”
This extraordinary surgical feat requires meticulous planning and three different specialized surgeons — a head and neck surgeon, a microvascular surgeon, and a maxillofacial surgeon — plus a prosthodontist and a biomedical engineer, the latter of which translates imaging data into a 3D model and creates patient-specific plates, guides, and implants.
An unusual program
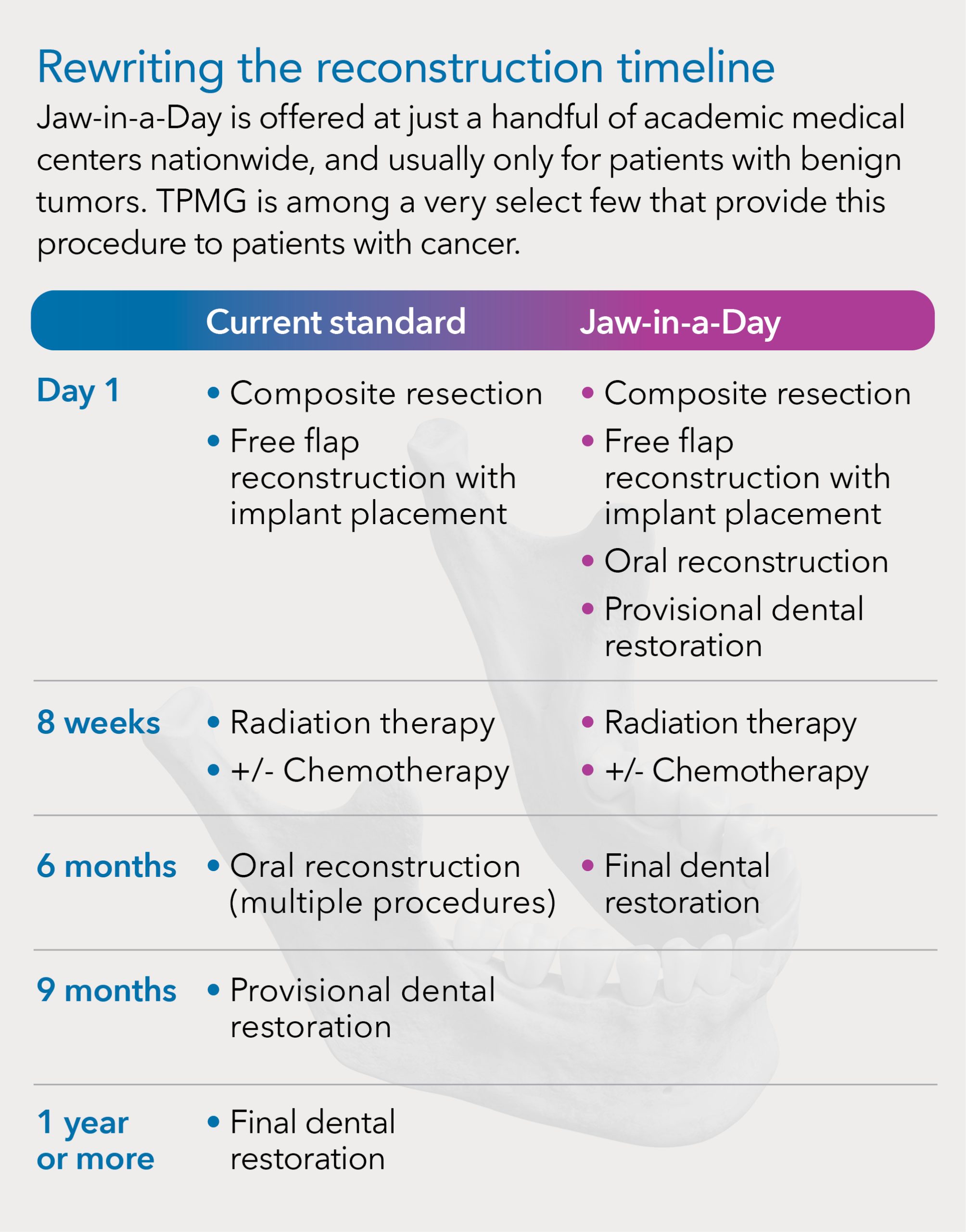
Jaw-in-a-Day is offered at just a small handful of academic medical centers nationwide, and usually only for patients with benign tumors. The Permanente Medical Group is among a very select few that also provide this advanced procedure to patients with cancer, who represent the largest group in need of this type of surgery in KP Northern California.
“To create and carry out a program like this is a tremendous accomplishment,” says Smita Rouillard, MD, TPMG associate executive director. “It takes real effort and courage to challenge the status quo and build something new. Our success reflects the dedication of these physicians, who believe in the mission of Permanente Medicine and who want to make care better for our patients.”
TPMG’s first Jaw-in-a-Day surgery took place in early December 2024, and that first patient’s reaction to the result has become a touchstone for the team at KP Oakland.

Heshaam Fallah, MD, DDS
“The day after surgery, I went to check on her during hospital rounds and found her in tears,” says Dr. Gurushanthaiah. “She explained that just moments before I walked into the room, she had finally looked in the mirror — and for the first time since childhood, she had teeth on that side of her smile. We had restored something she thought was lost forever. It was a really touching moment, and a reminder of the impact of our work.”
“I can’t emphasize enough how this surgery makes patients feel whole again,” says Heshaam Fallah, MD, DDS, chair of oral and maxillofacial surgery and chief at KP Oakland, who has been a key driver of bringing Jaw-in-a-Day to TPMG. “You might think it’s a small thing — it’s just teeth. But teeth are psychologically empowering.”
The traditional standard of care
Across the country, the standard care pathway for patients undergoing ablative and reconstructive jaw surgery is very similar to what the team’s first Jaw-in-a-Day patient experienced as a teen.

Daniel Sukato, MD
“Traditionally, a head and neck surgeon will resect the jaw and a microvascular surgeon will reconstruct it, usually using a fibula free flap, in a single operation,” says Daniel Sukato, MD, facial plastic and reconstructive surgeon and microvascular surgeon at KP Oakland. “If the patient has cancer, six to eight weeks later, he or she will undergo radiation and possibly also chemotherapy. Three to six months after that, patients have a second surgery, in which a maxillofacial surgeon exposes the fibula flap, places titanium implants, and then closes things back up.
“Another three to six months later, the patient has a third surgery, in which the fibula flap is re-exposed to put posts into the implants,” Dr. Sukato continues. “And then anywhere from three months to a year after that, the prosthodontist places a provisional dental prosthesis onto the posts, which is later replaced with a permanent prosthesis. Sometimes it can take a year for patients to get prosthetic teeth, sometimes two years, and sometimes, for a variety of reasons, it never happens at all.”
Within TPMG, advancements had already been made prior to introducing Jaw-in-a-Day to accelerate this timeline and improve the likelihood of a successful oral reconstruction, thanks to Dr. Fallah.
“One of the first things I did when I joined TPMG 14 years ago is to introduce the practice of inserting dental implants into the fibula flap during the initial reconstructive surgery, instead of several months later in a separate procedure,” he says, adding that this is something he learned during training and is now becoming more common nationwide. “This approach has been shown to have better, more predictable results. It’s especially beneficial for patients with cancer because placing implants after radiation therapy, as is done in the traditional method, causes a higher failure rate and potential loss of the jaw reconstruction.”
Drawbacks of a prolonged timeline
Although the practice of delaying and staging the rest of the oral restoration is designed with the best intentions — to give the jaw and vascular reconstruction time to heal — it comes with a set of risks and challenges that render outcomes unpredictable.
“Every time you do an additional surgery and re-expose a jaw reconstruction to the hostile environment of the mouth, which is full of bacteria, you’re risking infection,” says Dr. Gurushanthaiah.
Furthermore, Dr. Fallah adds, “Once scarring takes place after the initial jaw reconstruction surgery, patients are not able to open their mouths as wide or as freely because of contracture. It is extremely difficult, and sometimes impossible, for oral surgeons to reconstruct and recreate this space once it is lost.”
Even when the oral space is sufficient for dental restoration, other factors can create an impasse.
“When we plan these surgeries,” Dr. Fallah says, “we plan for the implants to project in a certain way to match where the teeth are, so that we can then build the dental reconstruction over them. However, if we don’t have a prosthesis in hand to verify that the implants are placed correctly, the angle of the implants could be off by a couple degrees or a millimeter or two, and we won’t know. This discrepancy can later make it impossible to create a prosthesis that fits and is functional.”
For patients with cancer, radiation therapy can cause tissue collapse, which can bury the implants and make dental restoration unachievable. And some patients, even though restoration is feasible, ultimately decide it’s not worth pursuing.
“Patients who go through cancer treatment are especially prone to getting what’s known as surgery fatigue, where they say, enough is enough,” says Dr. Fallah. “They’re like, I don’t want to go through multiple additional procedures to ultimately get teeth. I’ll just live with it.
“In the meantime,” he continues, “they’re suffering. Losing segments of dentition results in difficulties with chewing, speech, and oftentimes lip incompetence, especially if it’s in the front. The lip will cave in or curl back into the mouth, and then patients can’t really seal their mouths. Patients can have drooling problems, and it can be physically disfiguring. This often causes depression, and it’s particularly troubling for patients during the first six to 12 months after surgery. That’s a long time to wait for a dental prosthesis.”
Introducing Jaw-in-a-Day
It was for all these reasons that Dr. Fallah was keen to bring Jaw-in-a-Day to TPMG and for Drs. Gurushanthaiah and Sukato to join him in the endeavor.
Jaw-in-a-Day is not a new concept, but the procedure has evolved significantly since British maxillofacial surgeon Iain Hutchison, BDS, pioneered the approach in 2007. What began as a largely manual, high-risk surgery has become a streamlined, digitally guided operation with excellent outcomes, thanks to enormous advances in computer-aided design and manufacturing, especially in the last few years.
“Surgical teams at a few different academic medical centers have developed and published protocols and case studies demonstrating that Jaw-in-a-Day can be performed safely and reliably using modern virtual surgical planning,” Dr. Fallah says. “A couple of these centers now offer courses detailing how they integrated the procedure into their hospital systems, to enable others to replicate the approach in their own institutions.”
 The three TPMG surgeons attended one of these courses last year, and then promptly got to work adapting the protocols for KP Northern California — developing workflows, training staff, engaging a biomedical technology company for virtual surgical planning and manufacturing, and contracting with prosthodontists at the University of California, San Francisco. The surgeons also opted to include patients with malignant tumors in the eligible patient population — something very few other organizations offer.
The three TPMG surgeons attended one of these courses last year, and then promptly got to work adapting the protocols for KP Northern California — developing workflows, training staff, engaging a biomedical technology company for virtual surgical planning and manufacturing, and contracting with prosthodontists at the University of California, San Francisco. The surgeons also opted to include patients with malignant tumors in the eligible patient population — something very few other organizations offer.
“Jaw-in-a-Day has traditionally been offered only for patients with non-cancerous tumors because of concerns that subsequent radiation treatment could cause the jaw reconstruction to fail,” says Dr. Sukato. “The vascularized bone graft is pretty fragile. The bone is getting blood supply through blood vessels that we stitch together with tiny sutures. Then to insert implants and a dental prosthesis, and for patients to start using it, followed by a blast of radiation: It’s a perfect recipe for potential complications.
“Jaw-in-a-Day has gotten much more precise, with superior technology available to plan and execute the operation,” he continues. “This precision, in combination with the expertise of our multidisciplinary team and our already outstanding outcomes of fibula free flap reconstruction at KP Oakland, made us feel confident we could successfully bring the procedure to TPMG for cancer patients and that the reconstructions would survive radiation therapy.”
TPMG became the first organization in the Bay Area to offer Jaw-in-a-Day for malignancies, thereby joining the ranks of a tiny handful of prestigious academic medical centers nationwide, such as Cedars-Sinai and the University of Pennsylvania. (To learn more about one of TPMG’s patients with cancer who underwent the procedure, see “A patient perspective” at the end of this article.)
Preparing for surgery
With Jaw-in-a-Day, every aspect of care is driven toward long-term success and performed with end restoration in mind — starting with patient selection. Patients with benign tumors are referred via maxillofacial surgery or head and neck surgery, and the teams confer to evaluate whether a patient is a good candidate — a decision determined by tumor size, anatomical extent, and location. For patients with malignant tumors, all cases are reviewed by TPMG’s multidisciplinary tumor board for head and neck cancer.
“We have nine head and neck oncologic surgeons in KP Northern California — four in the East Bay, three in South Sacramento, and two in Santa Clara — and we meet every week to evaluate new cancer cases and discuss the best course of treatment,” says Dr. Gurushanthaiah. “If we determine that a patient is a good candidate for Jaw-in-a-Day, then we assemble the surgical team.” For most Jaw-in-a-Day cases thus far, the surgical team has consisted of Drs. Fallah, Gurushanthaiah, and Sukato, but other surgeons at KP Oakland have recently begun participating, and head and neck surgeons from other facilities, such as Bryan Fong, MD, from KP Walnut Creek, have come to Oakland for a few cases, as well.
After assembling the team, the next phase is advanced imaging and virtual surgical planning.
“The patient gets fine-cut CT scans of their jaw and lower extremities so that we can assess the bones and vascular supply,” says Dr. Gurushanthaiah, adding that patients don’t need to travel to Oakland for this — imaging can be done at the nearest KP medical center. Patients also meet with Dr. Fallah and receive an intraoral scan to capture images of their native teeth and tissue. This dental anatomy scan is then merged with the CT data.
“We import these scans into a 3D modeling system, and all three surgeons then sit down with the prosthodontist and a biomedical engineer to virtually resect the jaw and plan the reconstruction,” Dr. Gurushanthaiah continues. “The head and neck surgeon determines where to make the cuts in the jaw and the direction and placement of the plate. The microvascular reconstructive surgeon determines where to make the cuts in the fibula and how to shape them to reconstruct the jaw defect. And the maxillofacial surgeon determines where the implants will go in the fibula.”
Dr. Sukato explains that this virtual 3D environment allows the surgeons to experiment for optimal outcomes.
“For example, I can cut the fibula in multiple ways and manipulate the pieces to test different configurations,” he says. “Once we’re happy with how the reconstruction looks, we add a virtual prosthesis, and how this all fits together can influence the shape of the final product.”
From planning to execution
Based on the team’s specifications in this virtual surgical planning session, the biomedical engineer then designs and manufactures the materials needed for the surgery — and delivers them within 10 to 14 days.
“These materials include the resection guides for the patient’s native jaw, cutting guides for the fibula with slots for the dental implants, and the custom-fit reconstruction plate,” says Dr. Gurushanthaiah, adding that all these are made of titanium. “We also receive full-scale models of the patient’s jaw based on their natural anatomy, the jaw after the resection, and the fibula pieces at the size they will be after we cut them, so that we can see how it all fits into place.”
The team also receives the patient’s temporary prosthesis, which is made of plastic resin.
“The primary function of the temporary prosthesis is to provide tissue support and facilitate speech,” says Dr. Fallah. “It’s not really designed for chewing — the teeth are a little bit shorter than the final ones to limit pressure on the reconstruction and the prosthesis. It allows the tissue time to adapt and settle down around the implant so that everything heals properly, and so that the patient can get a final prosthesis that will fit comfortably and be fully functional.”
Practice makes precision
During the surgery, which takes approximately 8 to 10 hours, the three surgeons operate in concert. Dr. Gurushanthaiah is both an oncologic and microvascular surgeon, so he can do either the resection or the free flap reconstruction, but when he works with Dr. Sukato, he does the ablative part of the surgery.
“We work simultaneously,” says Dr. Gurushanthaiah. “So while I’m doing the tumor resection, Dr. Sukato is raising and shaping the flap, and then Dr. Fallah puts in the implants. If we time it perfectly, when I’m finished with the resection, they’re ready to bring the reconstruction done at the leg up to the jaw.”
The mechanics of the reconstruction are astonishing — everything fits into place with laser precision, thanks to virtual surgical planning and the expert team of surgeons.
“We remove a central segment of the fibula using the cutting guide created during surgical planning, with the bone still attached to the blood supply in the leg,” says Dr. Sukato. “Then, using slots in the guide, Dr. Fallah drills into the fibula flap and screws the implants in place. Next, we cut the fibula flap into smaller segments and reshape it at the leg — fitting the fibula pieces into the 3D model of the patient’s jaw. We then use the provisional dental prosthesis to confirm that the reconstructed segments are correctly aligned. Once the orientation is verified, we lock everything into place with the reconstruction plate.”
Dr. Fallah then indexes the prosthesis to the locked reconstruction — precisely aligning and recording its position for final placement.
“When we’re happy with how it all looks, we disconnect the blood vessels at the leg and go into ischemia time, at which point there’s a lot of pressure to finish the operation as quickly as possible,” Dr. Sukato continues. “We have the donor blood vessel ready to go, usually one of the facial arteries. We fit the reconstruction into place at the jaw and attach the plate, and once everything looks good under the microscope or high-magnification glasses, we suture the blood vessels together. This all happens ideally in under 2 to 3 hours.”
The last step is to deliver the prosthesis into the mouth, where it seats onto the implants exactly as planned.
A well-supported recovery
Dr. Gurushanthaiah explains that patients’ recovery time is variable, depending on how extensive the tumor is and whether any complications arise, but that patients generally spend about a week in the hospital while their jaw and leg heal.
“Patients don’t always need a tracheotomy for this surgery, but they do need a feeding tube because we’re exposing the mouth to the neck,” he says. “The surgical site needs to heal before they can start eating again, otherwise they could form an infection or get breakdown of the lining inside the mouth. It also takes a couple weeks for patients to be able to bear full weight on their leg.”
For patients with cancer, radiation therapy begins six to eight weeks after surgery, and patients may also work with specialists in dietetics, occupational therapy, physical therapy, and speech language pathology, depending on their individual needs. Three months after completion of radiation therapy, patients meet with the prosthodontist to be fitted for a final dental prosthesis, which is made of zirconium. The head and neck surgeon then follows the patient for five years, after which the patient is deemed cured if they do not have a recurrence.
Since performing their first Jaw-in-a-Day case, the team at KP Oakland already has conducted nine of these surgeries — all but two of them for patients with cancer — with superb outcomes. Drs. Fallah, Gurushanthaiah, and Sukato are providing training to colleagues in their respective departments to perform Jaw-in-a-Day to help spread the expertise in their medical center. The team is also teaching residents in head and neck surgery and maxillofacial surgery at KP Oakland to conduct this surgery.
“We follow the motto of ‘see one, do one, teach one,’ for our residents,” says Dr. Fallah. “So the residents observe first, and then we’ll go through with some guidance and have them do some parts of it. As they demonstrate more competency, we’ll let them to do a little bit more, with us still very much involved and hands on.”
Dr. Sukato adds, “It’s so important to teach younger physicians because they’re the ones who will be taking the care we currently provide to the next level in the future. We all like to say that we do excellent surgery, but at the end of the day, we are standing on the shoulders of all those who came before us. The progress we see today is built on generations of learning and refinement.”
Physician-led from start to finish
All three surgeons credit the organization’s multidisciplinary, integrated structure, support from TPMG physician leaders, and exceptional team collaboration for the success of this program.
“Our maxillofacial surgery division and head and neck surgery division are all part of one department, which means that we sit just a few doors down from one another,” Dr. Sukato says, adding that this is highly unusual. “This proximity, combined with our strong team rapport and long history of collaboration, has made it so much easier to develop the Jaw-in-a-Day program and choreograph this surgery.”
“Our team is also very humble and down to earth, and we all have the same goal: to do what’s best for patients,” adds Dr. Fallah. “I’m incredibly proud of the way we worked together to push the envelope and think creatively about how to accomplish something as special as this. And I’m grateful to our leadership, who supported us in bringing this to the organization so that we can provide optimal care.”
Dr. Gurushanthaiah agrees. “For us, it truly is all about the patients,” he says. “They go through so much with this cancer and with the treatment for it. And now, we get to tell patients that even though they have this life-threatening disease, not only are we going to remove the cancer and hopefully save their life, but we’re also going to rebuild them so that they’ll look pretty much normal afterward. To be able to give that to someone is a gift to us, too.”
This article originally appeared in Permanente Excellence, the magazine for physicians in The Permanente Medical Group.