A simple mantra — Reward Efficiency, Set Priorities, Empower Teams — helped Stacy Fletcher, MD, build a program that’s reinvigorating the practice of adult and family medicine in KP Northern California.
August 12, 2025
On an overseas flight in 2017 back to Germany, where she was stationed in the U.S. Air Force, Stacy Fletcher, MD, FAAFP, sketched out a concept on a cocktail napkin. This was nothing out of the ordinary, for she often doodles. “I’m a messy free thinker,” she jokes.
Dr. Fletcher had just attended two family medicine conferences in the United States, one for practicing physicians and the other for health care administrators. Both groups appeared depleted: Administrators were struggling to boost patient access and outcomes, and primary care physicians felt overwhelmed by numerous daily demands.

Stacy Fletcher, MD, FAAFP
On that long flight, she wondered, why it hasn’t been possible to achieve good outcomes and have happy staff? “I was illustrating ideas, thinking, there must be a better way — I refuse to accept that we can’t have both,” Dr. Fletcher says.
Those doodles at 30,000 feet were the beginnings of a new practice model at the Ramstein Air Base in Germany, where she was the medical director of the largest U.S. family health clinic overseas.
Fast forward to the present, and Dr. Fletcher has since adapted and implemented RESET (Reward Efficiency, Set Priorities, Empower Teams) in The Permanente Medical Group, where she has been practicing adult and family medicine at the Kaiser Permanente Vacaville Medical Center since 2018.
Dr. Fletcher describes RESET as a handshake agreement between frontline physicians and leadership that focuses on providing autonomy to frontline teams while improving critical clinical measures. It features a scorecard to track and measure these outcomes, as well as access to care, timely appointments, efficient scheduling, and patient satisfaction.
For participating TPMG adult and family medicine physicians, the voluntary program rewards strong results with increased autonomy. Those who choose to complete RESET training and subsequently achieve consistently high outcomes on their scorecards gain a high degree of autonomy in how they design their schedules, set their hours, and manage other aspects of their practice.
Today preventive care metrics for participating RESET teams within TPMG are higher than their counterparts’ traditional practices across all clinical measures, including cancer screenings, blood pressure, and diabetes control, and utilization is lower for resource-intensive services, such as emergency department visits, labs, and advanced imaging. In addition, access to care on RESET teams has improved significantly, and patients are much more likely to see their own physician over 90% of the time.
“The overarching goal,” Dr. Fletcher says, “is to create a private practice mentality and the best of both worlds — the flexibility and ownership mindset of independent practice within our amazing large, integrated health care system.”
A new approach to burnout
Signs of strain on the primary care workforce nationwide have been easily observable for quite some time now — since well before the pandemic. And there hasn’t been much convincing evidence that things are improving. According to Commonwealth Fund data from last year, nearly half of primary care physicians still report feeling burned out, and among those physicians, a whopping 39% say they plan to stop seeing patients within the next three years.

Christopher Walker, MD
Christopher Walker, MD, former physician-in-chief for the Napa-Solano service area and now TPMG associate executive director, says that time constraints and patient care pressures have only escalated in recent years as patients have become sicker and their care more complex. Meanwhile, physicians also juggle the demands of the electronic medical record system and its related inbox, which seems to have no bottom.
“Physicians aren’t able to get everything done during the workday that they need to get done, so they end up sacrificing personal or family time,” Dr. Walker says. “And then the work stacks. I would call it the hydra — you cut off four heads in one day, and you grow four more the next.”
RESET shows promise in that it provides a training curriculum aimed at encouraging physicians and their teams to think outside the box about scheduling and productivity in a way that improves patient access and care, while relieving stress and workload for the health care team.
The eight-month training includes three full-day, inperson sessions that follow a mountain-climbing analogy, in which each phase builds on the last. Participants progressively master key skills — such as reviewing schedules to identify patients who can be brought in for earlier care, conducting efficient outreach efforts, and achieving scorecard proficiency — before advancing to the next level.
Strengthening physician-MA teams
The program is designed to include medical assistants, so each physician-medical assistant team completes the ascents together, beginning with the training kickoff and continuing until they reach the summit at the end. During that stretch, the team also benefits from nearly 20 hours of individual coaching, Dr. Fletcher says.
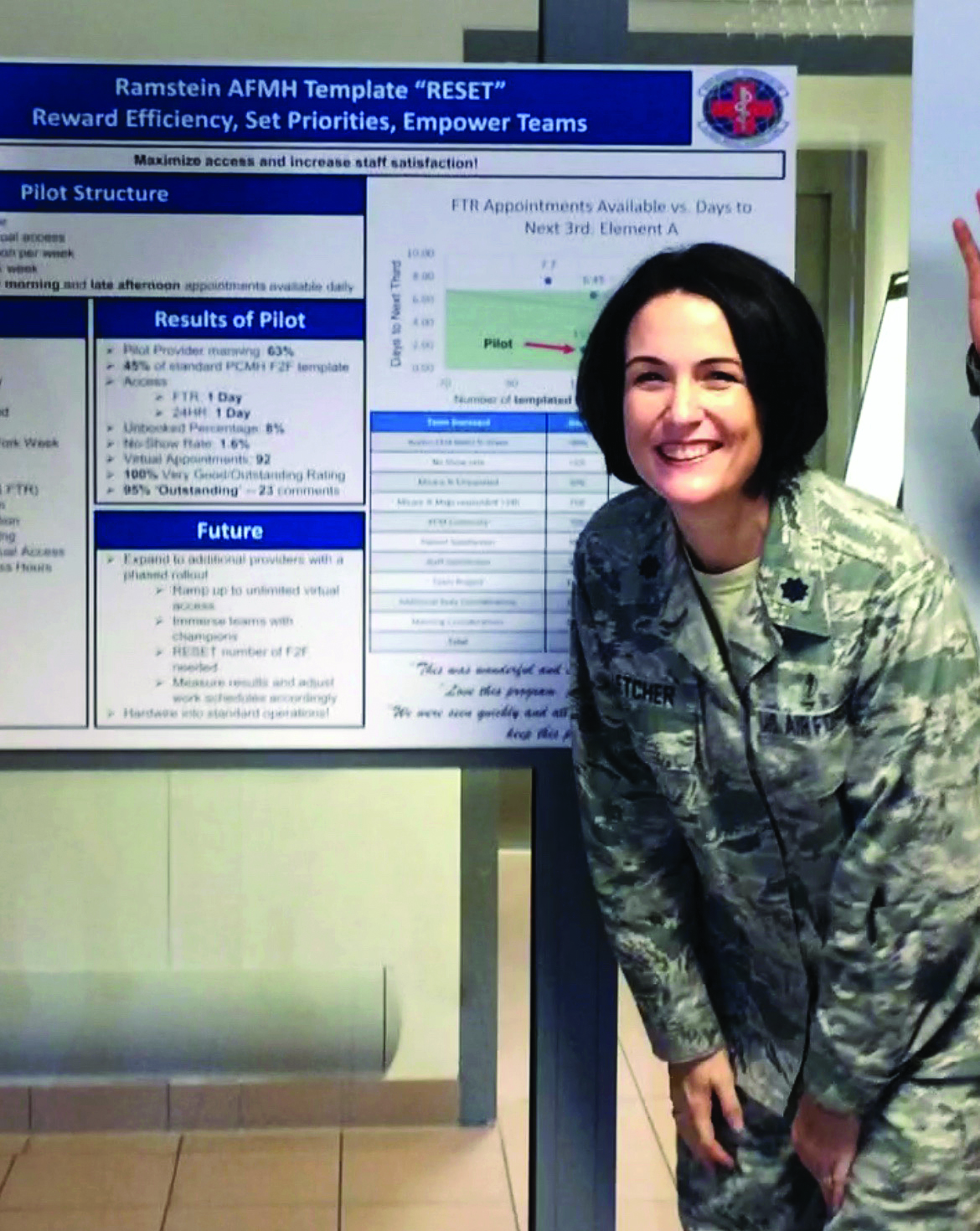
Dr. Fletcher stands in front of her poster presentation detailing the results of a RESET pilot at the Ramstein Air Force Base in Germany, during active duty in the U.S. military prior to joining TPMG.
“There’s a lot of focus on fun and creativity during trainings, including themed events, friendly competitions between teams, and related trophies,” says Khiem Nguyen, RESET program manager in TPMG.
“The medical assistants love it — they stay in communication with their doctor throughout the day and can directly book patients into the schedule,” adds Dr. Walker. “The physician and medical assistant work together to maintain access and quality of care, and they share a scorecard, so they either succeed or don’t succeed on the outcomes measures as a pair.”
Dr. Fletcher didn’t join TPMG in 2018 planning to implement her RESET approach. She had just left behind 17 years of active duty in the military — she remains part of the Air Force Reserves but was ready to shift gears a bit. “My plan was not to do RESET and instead spend whatever extra time I had raising my kids,” she says.
But soon, she couldn’t help but notice or ignore that the Vacaville Medical Center had some of the same issues she experienced during her Ramstein Air Base days, among them the struggle of adult and family medicine physicians against burnout amid productivity pressures and long lists of metrics.
“The problem is that I really have a heart for efficiency and for care teams being satisfied in their work,” she says.
A savvy partner
Dr. Walker, whom Dr. Fletcher has known since her days as a third-year medical student when they were stationed together, lobbied for her to build a RESET model in TPMG. For about six months, she resisted, in part because of the organization’s size and the related complexities of implementing the model. She would need a strategic partner, she told TPMG leaders, to consider moving forward.

Dr. Fletcher and RESET co-creator Andrew Muck are all smiles at a RESET training event in the Central Valley.
“I needed someone who could be emotionally intelligent and facile with data,” Dr. Fletcher says. “A good thought partner and someone who could be a little bit contrarian, so that they could challenge my sometimes wacky ideas.”
She drew up a purposely daunting list for Dr. Walker of key characteristics. “I gave him a list a mile long thinking, ‘Oh, that’ll do it. Now I won’t have to do this.’”
Shortly afterward she was introduced to Andrew Muck, MPH, whom Dr. Fletcher describes as crucial to the success of RESET. “He’s been an absolutely brilliant strategic partner — we are attached at the hip, and I can’t imagine doing this work without him.”
Their first meeting, scheduled for half an hour, stretched to three hours. Mr. Muck, director of strategic projects in the Napa Solano service area and regional director of RESET, was initially both intrigued and a bit skeptical.
“This idea of getting to a place where employees and physicians were more engaged, and that this engagement would drive better physician and staff performance — that part made total sense to me,” he recalls. But he wondered if moving away from more standardized processes, in the pursuit of more autonomy, would erode organizational performance and patient outcomes.
The more he worked with Dr. Fletcher, however, the more he recognized the brilliance of the approach. Together, with input from stakeholders, they co-created RESET for TPMG.
“The goal of the program has always been to achieve a true win-win-win, in which the work feels better to our frontline teams, we’re achieving organizational outcomes, and we’re improving the patient experience,” says Mr. Muck.
Addressing patients’ needs sooner
RESET launched as a small pilot in the KP Vacaville Adult and Family Medicine Department in March 2020. Despite the emergence of the COVID-19 pandemic that same month, leaders decided to move forward with the pilot, devoting nearly a year to assessing and refining the model before expanding to other service areas.
Key to RESET is a 23-metric scorecard that measures clinical outcomes, such as diabetes control and cancer screenings, as well as patient satisfaction. It also tracks access to care, including how often a patient can get in to see their personal physician, and how long it takes to get an appointment. One of the prime goals of the program is to keep 80% of appointments open for the following week.
“RESET training shifts each team’s mindset and incentivizes them to address patients’ needs sooner, if feasible, and thereby keep more future appointments open,” Dr. Fletcher explains.
Rather than booking all patient appointments for the same length of time — the traditional model for primary care — physicians and medical assistants can flex appointment length based on each patient’s needs. Or they may decide they can address the patient’s medical concern more quickly with a phone call or a video visit.
To achieve this, teams are trained to “handle today’s work today,” Dr. Fletcher says. “As they get that mastered, we teach them to do tomorrow’s work today. We teach them to find appointments that are booked out in the future that could be handled now.”
If a patient with back pain has booked an appointment in two weeks, for example, Dr. Fletcher or her medical assistant might reach out to see if the patient wants to come in sooner. “Not only does he get in sooner, but he also feels noticed, he feels seen,” she says. “He feels like his doctor is on top of things.”
Charting success
Since expanding the program to all adult and family medicine departments across the region, results have been impressive. Physicians who use the approach are seeing their patients 4.9 days sooner on average — within 6.2 days compared with 11.1 days previously.
Physician-medical assistant teams have the option to leave the program, or, if they are unable to pass their scorecard metrics after several attempts, they return to the traditional practice approach, Dr. Fletcher says. To date, 95% of TPMG physicians given the option have chosen to try RESET, and the two-year retention rate is 85%.
More than 2,800 adult and family medicine physicians and medical assistants in TPMG are participating in RESET. By year’s end, the remaining 1,200 physicians and medical assistants will have the option to enroll. Participation will remain voluntary, says Dr. Fletcher. Feedback from physicians so far has been overwhelmingly positive across the organization.
For internal medicine physician Rohini Ashok, MD, because RESET has enabled her to reengage with what she relished about patient care, she has postponed her plans to retire this year.
“Our jobs were getting extraordinarily stressful — this program literally reset everything,” says Dr. Ashok, who practices at KP San Jose. “I can take care of my patients the way that I want. We’ve been able to exhale, put the brakes on, and reconfigure our practices.”
Given longstanding relationships with patients that extend back decades, she continues, not every medical concern requires an in-person visit, and can sometimes even be handled via secure message. “We’re able to devote time now — time that we didn’t have before — to patient outreach and really focus on prevention,” she says.
Incorporating flexible scheduling
Yolanda Backus, MD, FAAFP, who was among the first physicians to complete RESET, relishes the flexibility to book appointments as long as 40 minutes to an hour that she knows will involve complexity, such as caring for transgender patients. Or she may need more time to meet the multiple needs of an older patient.
“You can’t cover seven things when you have 15 to 20 minutes,” says Dr. Backus, a family medicine physician at KP Davis. “Now that I can flex the appointment length based on the patient, I can address everything in one visit, and patients don’t have to keep coming back.”
Hyma Jasti, MD, chair of adult and family medicine in TPMG, has witnessed the benefit of RESET not only as a leader, but also in her own practice.
“What really impressed me when we first heard about RESET was the autonomy and the flexibility this program gives to the physicians so that they can both enjoy their work and do the right thing for patients,” says Dr. Jasti.
As with other teams using RESET, Dr. Jasti looks for opportunities to “scrub” her schedule, keeping as many appointments open as possible for the following week. She may call up a patient who has already booked an appointment for a troublesome rash for the following Monday. “I’ll say, ‘Can I help you today? You don’t have to wait until Monday.’”
RESET is effective, Dr. Fletcher explains, because it enables physicians to pursue outcomes goals that improve patient care, and at the same time reconnect them with why they chose medicine in the first place.
To illustrate, she tells a story about one of her own patients, someone who rarely comes in for care. Dr. Fletcher wanted to make sure that the patient completed her preventive screenings, including for cancer, in part as they’re tied to the outcomes scorecard. The patient’s appointment was at 10:30 a.m. and, as it turned out, an 11 a.m. mammogram slot had opened. Dr. Fletcher walked her down the hallway afterward for the screening test.
The patient was overwhelmed by the gesture. And when Dr. Fletcher left that day, she felt a sense of satisfaction. “I definitely benefited as much as she did,” she says. “I walked out and thought, ‘I was such a good doctor today.’”
Life and medicine — a delicate balance
To lead the expansion of RESET, Dr. Fletcher made a hard decision to step back from surgical obstetrics, a part of her practice that she loves and worked hard to train for with an advanced fellowship. “I look at it as a short-term break from delivering babies in order to deliver this baby,” she jokes.
Outside the office she’s also raising three children, ages 15, 14, and 10, juggling their various activities with her husband. She enjoys breaking away to camp on a piece of land that they purchased near Lake Oroville. “We love getting away and hunkering down as a family,” says Dr. Fletcher, who grew up in a military family and moved more than a dozen times in her early years. She will retire from 24 years of military service this fall with the rank of Colonel.

Dr. Walker celebrates with Dr. Fletcher at the ceremony honoring her as one of the recipients of the 2025 Sidney Garfield Exceptional Contribution Award.
Other initiatives Dr. Fletcher has spearheaded during her time with TPMG include the incorporation of a documentation tool within KP HealthConnect called Problem List Pro (PLP), which creates a synopsis of the patient’s health issues so that clinicians can spend less time hunting for key information and focus more on patient care. To date, roughly 1,800 physicians use it, she says. Her team is now teaching classes on combining the PLP approach with Abridge, a new ambient listening technology.
Dr. Fletcher also took her insights related to efficiency hacks and other productivity tools on the road last summer with other like-minded TPMG colleagues. They led what they dubbed The Grassroots Roadshow, a 1970s-themed series of training sessions that reached more than 800 physicians.
Dr. Fletcher, who won a Sidney Garfield Exceptional Contribution Award for this work earlier this year, credits the various teams she’s worked with through the years for making RESET and other productivity and outcomes-driven projects possible.
“I hate working alone,” she says. “Life and medicine are a team sport. I love that I have a fabulous team.”
For now, Dr. Fletcher is laser focused on wrapping up RESET’s rollout by year’s end. “As much as it’s hard work, it’s pretty darn fun,” she says.
“For leaders to see that not only are our outcomes getting better, but our clinical teams are happier — you can feel the weight coming off their shoulders. It’s an incredible privilege to know that we’re putting passion back into people’s work, creating sustainability for the organization, and dazzling patients. I’m honored to be at the tip of the spear doing this work.”
This article originally appeared in Permanente Excellence, the magazine for physicians in The Permanente Medical Group.