April 11, 2022
Kaiser Permanente study finds patients in low-socioeconomic-status neighborhoods benefited from help connecting with video medical visits
Patients participating in video visits with their primary care doctors in fall 2020 benefited from having a medical assistant help connect the call, particularly if they needed language interpretation or lived in a low-socioeconomic-status neighborhood, according to Kaiser Permanente research published April 11 in JAMA Internal Medicine.
“The involvement of a medical assistant seemed to reduce the technology gap,” said senior author Mary Reed, DrPH, a research scientist with the Kaiser Permanente Division of Research. “Our study didn’t identify exactly how this happens, but we believe it is because the medical assistant is available to walk patients through the technology and provide encouragement and a human connection.”
Kaiser Permanente Northern California, whose 9,500 physicians treat 4.5 million members, saw a rapid increase in the number of video visits in March 2020 as in-person medical care was reduced to limit COVID-19 virus transmission. In response, The Permanente Medical Group developed a regionwide initiative to promote and support video care. This initiative included the practice of “virtual rooming,” which involves a medical assistant (MA) calling the patient 15 minutes before the visit to help connect the video call.
The study’s authors looked at trends in October 2020, comparing medical offices that used virtual rooming more with those that used it less. They found that virtual rooming increased connection rates for all patients. Patients of medical offices with high virtual rooming rates were 7% more likely to have a successful connection.
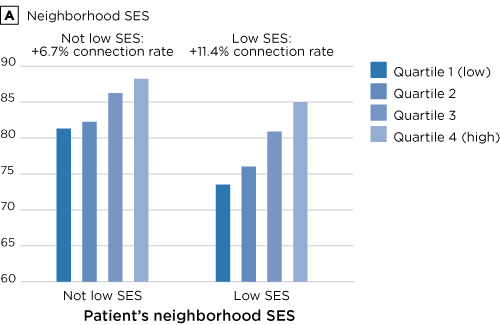
Video visit connection rates by high vs. low virtual rooming, and neighborhood socio-economic status (SES).
In general, some patients were less likely to make a successful video visit connection: those needing language interpretation, those living in a low-socioeconomic-status neighborhood, Black patients, and Latino patients. However, medical assistant involvement helped reduce this gap.
After adjusting for patient factors such as age and comorbidities, estimated connection rates with MA assistance were 11.4% higher for patients who lived in low socioeconomic status neighborhoods. Increases were 12.1% for Black patients, 9.8% for Latino patients, compared with 8.1% for Asian patients and 5.2% for white patients. For those needing language interpretation, connections with assistance were an estimated 13.1% higher, compared with 7.4% for those not needing interpretation.
Overall, the study found 87% of video visits had a successful connection, “which is stellar in my opinion,” Reed said. “There’s always a chance that technology will fail or you won’t have good enough reception. We found a very high rate of success during a challenging time of the pandemic.”
How virtual rooming works
As virtual visits skyrocketed during the pandemic, Kaiser Permanente clinical leaders in Northern California recognized that medical assistants could have an important role to play, explained Christine Levan, MD, regional director of performance improvement in primary care. “Working with our physicians and staff, we built and tested an effective workflow at one facility and then shared it throughout the region,” she said.
The process included training for both medical assistants and clinicians, with updates as new and better methods were identified — such as texting the patient a link to the video meeting. “We wanted virtual rooming to roll out consistent with our values of safety, compassion, integrity, excellence, and efficiency,” she added.
Along with helping with technology, medical assistants also determine the patient’s main goal for the visit and whether preventive care or screenings are needed. “Virtual rooming is really powerful because medical assistants have the chance to connect with patients in their homes,” Dr. Levan said. “To see the actual evidence and data of these benefits was remarkable and validating.”
Kaiser Permanente generated weekly reports on virtual visits, which included the medical assistant rooming rate and video connection rate. These reports were shared widely and prompted local leaders to share best practices with one another to improve processes.
“We found a lot of creativity in how clinicians and medical assistants adjusted workflows to make this transition to virtual care work well for patients,” said lead author Tracy Lieu, MD, MPH, director of the Kaiser Permanente Division of Research. “This research draws attention to the very important role of medical assistants in our virtual as well as in-person care. They are particularly important for those patients who may need a little extra help bridging the digital divide.”
The study was funded by The Permanente Medical Group’s Delivery Science and Applied Research Program.
Additional co-authors were E. Margaret Warton, MPH, and Loretta Hsueh, PhD, of the Division of Research; and Karen San, MS, and Sameer Awsare, MD, of The Permanente Medical Group.
This article originally appeared in Division of Research Spotlight.