January 2, 2024
Specialized prompts integrated into patients’ electronic medical records can improve how medical oncologists discuss and document treatment goals for their advanced cancer patients, new Kaiser Permanente research published in the American Journal of Hospice and Palliative Medicine shows.
Ashley Aller, MD
“Giving patients a voice in their care is every physician’s priority,” said first author Ashley Aller, MD, a delivery science oncology research fellow at the Kaiser Permanente (KP) Division of Research and a hematology and oncology fellow at KP Northern California. “We know that when goals of care discussions are conducted well, they can improve a patient’s quality of life, increase patient and family satisfaction, lower costs, and reduce nonbeneficial care.”
KP Northern California had previously added a Life Care Planning Navigator that contains palliative care provider notes and Physician Orders for Life Sustaining Treatments (POLST) forms to its electronic medical record system to document patients’ end-of-life treatment preferences. However, the provider notes don’t always clearly document a patient’s personal treatment goals.
To help oncologists identify and amplify their patients’ goals, the research team developed a new online prompt, “What Matters Most/Quality of Life.” In a pilot program, the researchers added the prompt to the Life Care Planning Navigator used at the KP San Francisco Cancer Center between January and May 2022. They found the prompts increased the rate of oncology provider goals of care documentation for advanced cancer patients from 9% to 47%, with 15 of the 17 eligible clinicians using the new guide to document their conversation.
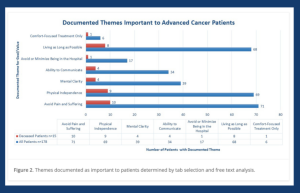 The new study analyzed the notes medical oncologists made using the new prompts in conversations with 178 advanced cancer patients. The study showed the most common reason oncologists initiated a goals of care conversation was related to the patient’s prognosis or a change in their medical condition. The most frequently documented goals of care were avoiding pain and suffering, physical independence, and living as long as possible. The least-recorded goal was avoiding or minimizing being in the hospital and comfort-focused treatment only.
The new study analyzed the notes medical oncologists made using the new prompts in conversations with 178 advanced cancer patients. The study showed the most common reason oncologists initiated a goals of care conversation was related to the patient’s prognosis or a change in their medical condition. The most frequently documented goals of care were avoiding pain and suffering, physical independence, and living as long as possible. The least-recorded goal was avoiding or minimizing being in the hospital and comfort-focused treatment only.
The study found that the prompts helped oncologists clearly identify patients’ treatment goals and that people, interests, or specific events — like a forthcoming birthday or graduation they hope to attend — motivated their decisions.

Raymond Liu, MD
“We worked with representatives of the cancer center’s patient advisory council to develop the prompts using patient-friendly language that would elicit information about not only what matters most to patients but how they define quality of life,” said senior author Raymond Liu, MD, an adjunct investigator with the Division of Research and director of research for the KP Northern California Hematology-Oncology Service Line.
The prompts made it possible for oncologists to document goals of care in a way that was uniquely focused on the patient. They also help oncologists provide context for the goals, values, and motivators the cancer care team should be aware of as they work with the patient to make decisions related to their treatment and care.

Aida Shirazi, PhD
“This research is exploring a new chapter in personalized cancer care,” said co-author Aida Shirazi, PhD, the lead senior project manager at the KP Northern California Department of Graduate Medical Education. “Amplifying the patient’s voice is a critical component of practicing medicine and is paramount in addressing health inequities and providing quality health care for all cancer patients.”
The researchers hope oncologists will use their findings to implement similar online prompts. “Our study highlights the importance of documenting these conversations and identifying what matters most to patients,” said Dr. Liu.
Added Dr. Aller, “This research was inspired by my grandmother, and the lessons she taught me as she was being treated for cancer. She would tell me her goals, and what motivated her, even when her cancer was advanced. She showed me how important it is to both ask and communicate individualized goals and values.”
Co-authors include Karen Hauser, MD, MPH, Jenny Wei, MD, Ali Duffins, MD, Jed Katzel, MD, Francisco Martinez, MD, and Amy Lin, MD, of Kaiser Permanente Northern California; Andrea Altschuler, PhD, of the Division of Research; Megan Cheslock, MD, of Edith Nourse Rogers Memorial Veterans’ Hospital; Hannah Whitehead, RN, MSN, Peggy Lim, MD, Tyler Jones, BA, and Sue May Yen, BS, MS, of The Permanente Medical Group; Steve Aller, MD, PhD, of Seattle Children’s Hospital; Cynthia Aller, DO, PhD, of Providence Regional Cancer System Lacey Cancer Clinic; and Leon Pedell, MD.
This article originally appeared in Division of Research Spotlight.






