November 20, 2024
Kaiser Permanente’s comprehensive, evidence-based tobacco screening and cessation program has helped more than 300,000 of its members in Northern California quit smoking since 2014, a new study shows.

Renee Fogelberg, MD
The research, published in the American Journal of Preventive Cardiology, found that the percentage of Kaiser Permanente (KP) Northern California members who reported smoking dropped from 8.6% in 2014 when the program was implemented to 5.8% in 2023.
“Our success is based on a multi-pronged approach that targets at-risk patients, provides low-cost or no-cost cessation therapy, and personalizes the care patients receive,” said lead author Renee Fogelberg, MD, an obstetrician-gynecologist with The Permanente Medical Group and the clinical lead for KP Northern California Tobacco Cessation. “We also have tobacco consultants in our medical centers who help drive performance, share best practices, and create visibility for this important initiative.”
State-of-the-art program

Jamal Rana, MD, PhD
Cigarette smoking is responsible for 1 of every 4 deaths from cardiovascular disease in the U.S. In 2021, about 11.5% (28.3 million) of U.S. adults reported being a current cigarette smoker.
“As a cardiologist, smoking is always of concern when it comes to our patients,” said senior author Jamal Rana, MD, PhD, an adjunct investigator with the Kaiser Permanente Division of Research and a cardiologist with The Permanente Medical Group. “Within our system we had an idea about the phenomenal work done by numerous teams for smoking cessation. Now, with this publication, we have shown that our interventions were associated with a statistically significant decrease in the prevalence of tobacco use.”
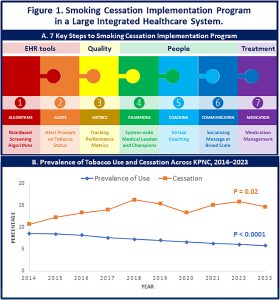
In 2014, KP Northern California updated its screening cessation program to incorporate new evidence-based interventions and implement methods for measuring long-term success. Critical to the program’s success is a risk-based algorithm built into the electronic medical record that screens every patient receiving care across 50 medical departments.
 Patients ages 13 to 17 are screened at every visit regardless of smoking history. Patients age 18 and older are screened at every visit if they are current smokers or have quit in the last year. People who have never smoked (never smokers) are screened every 2 years. This results in about 250,000 screenings per month, including 800 screenings during pre-surgery appointments.
Patients ages 13 to 17 are screened at every visit regardless of smoking history. Patients age 18 and older are screened at every visit if they are current smokers or have quit in the last year. People who have never smoked (never smokers) are screened every 2 years. This results in about 250,000 screenings per month, including 800 screenings during pre-surgery appointments.
Patients who are current smokers are offered information on a range of smoking cessation options. This offer is repeated by phone or via email. The study found that the comprehensive program resulted in 0.34% annual decrease in the prevalence of smoking and a 0.41% annual increase in the percentage of current smokers who quit from 2014 to 2023.
Patient-focused approach
“Our success in helping members quit smoking can be attributed to this coordinated and patient-focused approach,” said co-author Kelly Young-Wolff, PhD, MPH, a clinical psychologist and Kaiser Permanente Division of Research investigator. “By embedding smoking cessation resources within routine health care practices, we ensure continuous engagement with our members regarding their smoking status. Also, by making care accessible and building in long-term follow-up, we create a supportive environment that contributes to sustainable success.”

Kelly Young-Wolff, PhD, MPH
As part of the program, patients who smoke are encouraged to get help quitting prior to surgery. Nicotine replacement therapy prescriptions are included in admission order sets so that smokers can be placed on medical therapy to address withdrawal symptoms they may experience while hospitalized. And pregnant patients who smoke are offered counseling with a licensed mental health clinician who specializes in prenatal substance use to assess their usage and help them abstain from tobacco and other drugs.
Kaiser Permanente also makes it easy for members to connect with experts in behavior change who work with physicians to tailor medical therapy. Physicians can refer patients to these experts, and patients can also self-refer.
“These interventions underscore our dedication to supporting our members in achieving smoking cessation and our proactive commitment to integrating cessation strategies into the broader health care system,” said Ms. Young-Wolff.
The study team believes similar programs could be applied across most health care systems. “We have highlighted the key steps that can unlock such success in other health care systems and practices,” said Dr. Rana.
Co-authors include Jaya Nadella, BS, of the Division of Research, and Mehreen Khan, MD, and Yi-Fen Irene Chen, MD, of The Permanente Medical Group.
This article originally appeared on Division of Research Spotlight.






